Cancer of penis and prostate
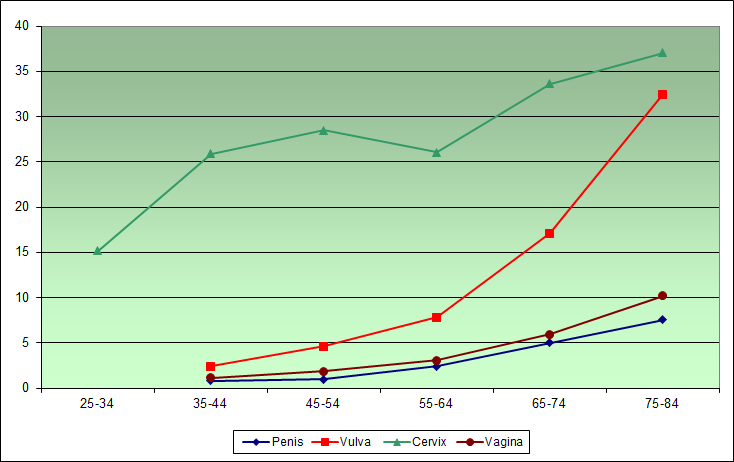
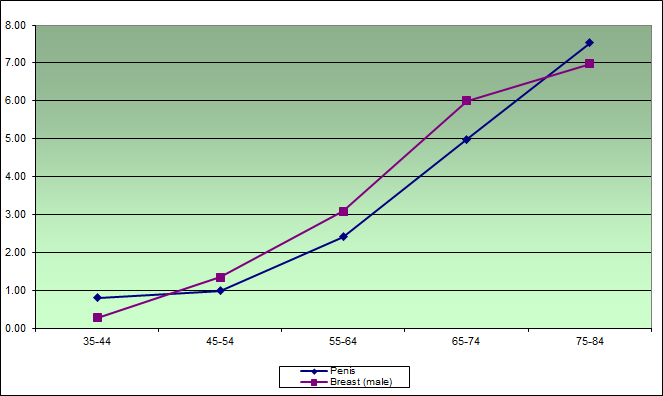
Cancer occurs when the mechanism controlling the replication of cells goes haywire and new cells proliferate beyond replacement level. The main causes of such malfunction are mutations to the DNA of the cell, usually caused by smoke, industrial chemicals or radioactive materials, and the effects of ageing, which increases the rate of copying errors as cells divide. The longer we live the more likely we are to get one form of cancer or another. Men are far more likely to get cancer of the prostate, lung, colon, bladder or exposed skin than of the penis, which is about the last place in the body where it is found. As the graphs below show, cancer of the cervix and vulva in females, as well as cancer in the male breast, is far more common than cancer of the penis - yet nobody proposes that we routinely excise female genital tissue or male breast tissue as a precaution against the risk of cancer in later life.
A very rare disease: Lifetime risk of cancer of the penis
The following is an excerpt from Professor Robert Van Howe’e lecture, “Math is Your Friend: A Consumer’s Primer to Understanding Epidemiology”
One of the statistics that is bantered about is the lifetime risk of acquiring certain illnesses. This cannot be calculated from prevalence because illnesses can come and go, afflict different people for different lengths of time, result in early death, or present at different ages. We can however calculate lifetime risk from incidence estimates. Since incidence estimates are age-adjusted, the lifetime risk is approximately the yearly risk multiplied by the average lifespan, which is 72 years. So for penile cancer in the United States, the lifetime risk would be 0.0000058 X 72 or 0.0004176 (The precise formula gives an answer of 0.000417512).
Lifetime risk is usually not expressed in this fashion because no one wants to count the number of zeroes following the decimal point, but as the inverse (1/x) of this number. In this case, the inverse is expressed as a one in 2395 lifetime risk. To put this in perspective the lifetime risk of breast cancer in women is one in eight. By comparison, penile cancer is a rare illness.
Number Needed to Treat
This can be taken a step further. The 2012 American Academy of Pediatrics Task Force report noted that you needed to circumcise 909 males for that one case of penile cancer. This estimate came from a discussion section of an article citing a 1980 opinion piece that assumed that it was impossible for circumcised men to get penile cancer.4 We now know that is nowhere near the truth. They also noted that a review article put this number at 322,000.5 The review article confused incidence with lifetime risk and failed to multiply it by 72 as discussed above. Neither number is correct. Interestingly, the Task Force had all the numbers at its disposal to make a rough estimate of the number needed to treat but failed to recognize this opportunity or act on it.
Let's do the math they were unwilling to do. The lifetime risk, as we noted above, is 0.0004176. The Task Force report noted that the relative risk reduction for penile cancer by circumcision was between 1.5 and 2.3. If you take the lifetime risk of penile cancer and reduce it by a factor of 2.3 you get 0.0001815, which would be the expected lifetime risk for penile cancer in circumcised men. The absolute risk reduction would be the difference between the two rates: 0.0004176 minus 0.0001815 or 0.0002360. The number needed to treat is the inverse (1/x) of the absolute risk reduction or 4237. This means that 4237 infant males would need to be circumcised in order to prevent one case of penile cancer, which usually strikes on average at 80 years of age. If, however, the relative risk reduction is 1.5, the number needed to treat is 7184.
Cost Effectiveness
So how much does it cost to prevent one case of penile cancer using infant circumcision? If it takes 7184 circumcisions to prevent one case of penile cancer and each circumcision costs an average of $285 paid at the time of the procedure,6 the cost would be the product of these two numbers or $2,047,440. But the story does not end there. The money for the circumcision was spent at the time the male was circumcised, but penile cancer usually does not develop until about 80 years of age. So, for 80 years the opportunity of having that cash spent at the time of the procedure has been lost. These opportunity costs add up over 80 years. For example, if that money were put out at 3% interest for 80 years, the opportunity costs would be $21,786,584. If the money were to earn 5% interest for 80 years, the costs of preventing one case of penile cancer would be $101,474,076. This may explain why the American Academy of Pediatrics Task Force elected not to do the calculations.
Source: Dr Robert Van Howe. Math is Your Friend: A Consumer’s Primer to Understanding Epidemiology
Cancer Council of Australia rejects circumcision
The Cancer Council of Australia has come out strongly against recent (2012) claims that mass circumcision of boys is necessary as a preventive of cancer of the penis and prostate. In a statement released on 21 June, the Council warned that cancer of the penis was a rare disease in Australia, and that the evidence of circumcision having a protective effect was not sufficient to justify the operation. As to prostate cancer, the main risk factor was nothing more than getting old - a natural process that circumcision could do nothing to arrest. The statement concluded: “Taking into account these issues, the relatively lower burden of potentially preventable disease in Australia, and the complex cultural, ethical and legal issues surrounding the practice of circumcision, Cancer Council Australia does not recommend circumcision as a routine cancer-preventive procedure at this time.”
Source: Cancer Council of Australia, Neonatal male circumcision and cancer
Further comment at Intactivists of Australia
Incidence and prevalence of cancer of the penis
Cancer incidence in Australia by age cohort, showing that cancer is a disease of ageing and that male breast cancer
is more common than cancer of the penis (cases per 100,000 per age-cohort)
According to the American cancer society (Cancer Facts and Figures 1996), the leading sites of cancer in males are:
prostate 317,100 cases
lung 98,900
colon and rectum 67,600
bladder 38,300
lymphoma 33,900;
melanoma 21,100;
oral 20,100;
kidney 18,500;
leukemia 15,300;
stomach 14,000;
pancreas 12,400;
liver 10,800.
Having listed prostate and testis separately, it listed “other and unspecified reproductive”. The projected number of cases of “other and unspecified reproductive, male” cancers for 1996 was 1,200. Even if we assume that these are all penile cancer cases – not all of which would be sited on or near the foreskin – that is a tiny fraction of all cancers. With a total of 649,100 cases of cancer in males, “other and unspecified reproductive” cancers in males amounted to 0.18% of malignancies.
Having listed prostate and testis separately, it listed “other and unspecified reproductive”. The projected number of cases of “other and unspecified reproductive, male” cancers for 1996 was 1,200. Even if we assume that these are all penile cancer cases – not all of which would be sited on or near the foreskin – that is a tiny fraction of all cancers. With a total of 649,100 cases of cancer in males, “other and unspecified reproductive” cancers in males amounted to 0.18% of malignancies.
The leading sites of cancers causing death are:
lung 94,400
prostate 41,400
colon and rectum 27,400
pancreas 13,600
lymphoma 13,600
leukemia 11,600
oesophagus 8,500
liver 8,400
stomach 8,300
bladder 7,800
kidney 7,300
brain 7,200
Projected deaths from “other and unspecified reproductive” cancers in males were 220. That’s 0.093% of the total cancer deaths.
Some of the rare cancers, apart from “other and unspecified reproductive, male” that men are more likely to get and perhaps die from, include: lip, tongue, mouth, pharynx, oesophagus, small intestine, larynx, bone, connective tissue, Hodgkin's disease, testis, and thyroid.
Male breast cancer amounted to 1,400 cases, with 260 deaths. This means that American men are more likely to suffer from and die of breast cancer than penile cancer. Why does nobody suggest neonatal amputation of a male’s useless breasts to protect him against this malignancy?
Australian figures
The figures are similar for Australia. The New South Wales Cancer Council reports that in 2005 four sites accounted for 63% of all new cancers in males. These were cancers of the prostate (31%), bowel (13%), melanoma (10%) and lung cancer (9%). The most common causes of male cancer deaths were lung (21%), prostate (14%) and bowel (13%).
The word circumcision does not appear on the website of the NSW Cancer Council.
Phimosis and cancer
There is some evidence that severe phimosis accompanied by poor hygiene increases the risk of cancer of the penis. The correct answer here is not circumcision, but treatment to correct the phimosis and regular washing.
Just why severe phimosis increases the risk of penile cancer is unclear, but it is possibly a consequence of the exposure of the skin to unwashed seminal secretions. Despite the persistence of such myths, the notion that sub-preputial moisture (“smegma”) is carcinogenic has been thoroughly debunked, but it is possible that chemicals in the seminal fluid could be carcinogenic over the long term. These have to be fairly lethal in order to protect the sperm from hostile antibodies in the female genital tract, which would otherwise kill such invaders before they could do their job. This might also explain why cancer of the prostate (where the seminal fluid tends to accumulate if not discharged regularly) is (relatively) so common.
Could circumcision cause cancer?
Some cases from Saudi Arabia, where nearly all boys are circumcised in accordance with Islamic custom, suggest that circumcision could increase the risk of cancer of the penis.
Seyam RM, Bissada NK, Mokhtar AA, Mourad WA, Aslam M, Elkum N, Kattan SA, Hanash KA.* Outcome of penile cancer in circumcised men. J Urol. 2006 Feb;175(2):557-61
PURPOSE: We previously reported on a group of patients with post-circumcision carcinoma of the penis. We now study the long-term outcome of these patients.
MATERIALS AND METHODS: We retrospectively reviewed the available charts of 22 patients presenting between October 1979 and May 2000.
RESULTS: Of 22 patients 18 underwent ritual circumcision with extensive scar development. Median age at diagnosis was 62.4 years. The penile lesion was dorsal and proximally located in 15 patients. Median delay before diagnosis was 12 months. Clinically 14 patients had stage T1-T2 disease, with 13 having no lymph node involvement and none with distant metastasis, 8 patients had stage T3-T4 disease. A total of 15 patients were treated surgically with total penectomy (10) or conservative local excision (5), inguinal lymph node dissection (9) and subsequent penile reconstruction (3). Pathological staging in 15 patients revealed 10 patients with stage T1 and in 8 patients with lymph node dissection none had nodal metastasis. Histopathological classification was 20 squamous cell carcinoma, 1 sarcoma and 1 verrucous carcinoma. Six patients refused surgery and 1 was referred for palliation. Median followup was 14.5 months and median survival was 14.5 months. The 3-year survival was 42% for stage T1-T2 and 13% for T3-T4 (p = 0.0052). Median survival for the surgical group was 34 months whereas for nonsurgical group was 3 months (p = 0.0016). Recurrence-free survival in the surgical group was 50%.
CONCLUSIONS: Penile carcinoma in circumcised men is a distinct disease commonly following nonclassic vigorous circumcision. Delayed diagnosis and deferring surgical treatment are associated with increased mortality.
* Department of Urology, King Faisal Specialist Hospital and Research Center Riyadh, Saudi Arabia. rmseyam@hotmail.com
J Urol. 2006 Feb;175(2):557-61
Read more about cancer of the penis at CIRP.
Read more about cancer of the penis at Circumstitions.
More information from Google Knowledge
Risk factors for cancer of penis do not include foreskin
The chapter on cancer of the penis in a new edition of an authoritative Oxford textbook on cancers points out that cancer of the penis is an extremely rare disease (in fact, less common than cancer of the male breast) and that the risk factors are preventable conditions, including pathological phimosis and infection with human papilloma virus. The foreskin is not a risk factor for cancer of the penis, and circumcision does not infallibly prevent it. The summary of the chapter follows:
Penile cancers are rare primary malignancies located on the glans, foreskin, or shaft of the penis,
excluding the urethra. The vast majority of penile cancers are epithelial tumors representing
histological subtypes of squamous cell carcinoma (SCC). Most penile SCCs are believed to develop
through preinvasive lesions known as penile intraepithelial neoplasia and penile carcinoma in situ.
Penile cancers account for 0.1%–0.3% of all incident cancers (excluding non-melanoma
skin cancers) in the United States and other developed countries and up to 1% of all cancers in some
countries in sub-Saharan Africa. Annual incidence rates per 100,000 men (world standardized) are
typically between 0.3 and 1.0 in developed countries, being 0.5 in the United States. During 2002–
2011, SEER data showed rather stable penile cancer rates with no statistically significant changes in
incidence or mortality.
Being rare in men younger than 40 years, penile cancers are typically diagnosed among men
above age 60. The 5-year relative survival rate after penile cancer was 67% for all stages combined
in US patients recorded in SEER registries during 2004–2010, with foreskin cancers having a more
favorable prognosis than cancers at other penile sites.
The two most important risk factors for penile cancer are pathological phimosis and
infection with high-risk types of human papillomaviruses (HPV), which are both preventable
conditions. Non-surgical strategies to reduce the frequency of pathological phimosis need
consideration, particularly because rates of newborn circumcision are declining in the United States
and elsewhere. Increased awareness among doctors and parents about the importance of non-interference
with the physiological foreskin separation process in young boys, and the promotion of
safe-sex practices, possibly combined with preadolescent gender-neutral HPV vaccination
programs, will likely reduce the frequencies of pathological phimosis and sexually acquired HPV
infections and, eventually, reduce the burden of penile cancer at the population level.
Source: Frisch M. 2018. Penile Cancer. In: Thun M J, Linet M S, Cerhan J S, Schottenfeld D (Eds.), Cancer Epidemiology and Prevention (4th ed., pp. 1029-1038). Oxford University Press, New York.
Smegma is not carcinogenic
Despite the importance of avoiding smegma so frequently stressed by enthusiasts for routine circumcision, there is no evidence at all that smegma is harmful. Why would it be? It's just a natural secretion like saliva, found in the genitals of both males and females.
The carcinogenicity of smegma: Debunking a myth
RS Van Howe,* FM Hodges‡
*Department of Pediatrics, Michigan State University School of Human Medicine, Marquette, MI and ‡Berkeley, CA, USA, in Journal of the European Academy of Dermatology and Venereology, Vol. 20, 2006, pp. 1046-1054
Abstract
Background: Smegma is widely believed to cause penile, cervical and prostate cancer. This nearly ubiquitous myth continues to permeate the medical literature despite a lack of valid supportive evidence.
Methods: A historical perspective of medical ideas pertaining to smegma is provided, and the original studies in both animals and humans are reanalysed using the appropriate statistical methods.
Results: Evidence supporting the role of smegma as a carcinogen is found wanting.
Conclusions: Assertions that smegma is carcinogenic cannot be justified on scientific grounds.
Extract from the conclusion
The evidence does not support the theory that smegma is a cause of genital cancer. The smegma theory of disease was best stated by Boczko and Freed: "Smegma, a sterol, produced by Tyson’s glands in the epithelium of the retroglandular sulcus, has been implicated as the causative agent. It may be converted to a carcinogen by the action of the Mycobacterium smegmatis." [69] From the medical literature we have found that smegma is not a sterol, that there are no Tyson’s glands, that smegma is not converted to a carcinogen by M. smegmatis, and that M. smegmatis is not part of the normal genital flora. The myth is sustained only by its popularity among circumcision advocates.
Some have extrapolated the smegma theory by hypothesizing that men with inadequate circumcisions may be at risk for cancer because smegma can accumulate under any foreskin remnants. [70] In similar fashion, Abraham Ravish expanded the smegma theory to indict smegma as the cause of prostate cancer by travelling upstream through the urethra to invade the prostate gland. [71] Davis-Daneshfar and Trueb speculated that chronic infection with M. smegmatis is the cause of plasma cell (Zoon’s) balanitis, [72] but Yoganathan et al. could not isolate the organism in any of their cases. [73]
Some have shown an unwillingness to abandon the smegma theory. When it was postulated that sperm proteins caused cervical cancer, it was the smegma mixing with the sperm proteins that were to blame. [74] When diaphragm use was found to decrease cervical cancer, it was postulated that it provided a barrier to contact with smegma. [75] When it was clear that cervical cancer resulted from a viral infection, some still postulated that smegma was a necessary part for the viral exposure to be carcinogenic. [45] Those promoting the ‘cocoon’ theory prefer to think of smegma as a cofactor in the development of penile cancer.
There are two reasons to dismiss this speculation. First, there is no scientific evidence to support the assertion. Second, it is analogous to declaring saliva a cofactor in the development of lip cancer in those who chew tobacco. Both saliva and smegma are bodily fluids that serve a function and, like any other bodily fluid, are present in organs than can develop a malignancy. The purpose of the scientific method is to distinguish between wishful thinking, strongly held pinion, and provable fact. The smegma theory of disease, which began as wishful thinking on the part of circumcision zealots such as Abraham Wolbarst and Abraham Ravich, has evolved into irrefutable dogma, but as modern physicians, we need to recognize that, until proved otherwise, smegma is harmless.
References
69. Boczko S, Freed S. Penile carcinoma in circumcised males. N Y State J Med 1979; 79: 1903–1904.
70. Culp D. Penile cancer. J Iowa Med Soc 1973; 63: 201–202.
71. Ravich A, Ravich RA. Prophylaxis of cancer of the prostate, penis and cervix by circumcision. N Y J Med 1951; 51: 1519– 1520.
72. Davis-Daneshfar A, Trueb RM. Bowen’s disease of the glans penis (erythroplasia of Queyrat) in plasma cell balanitis. Cutis 2000; 65: 395–398.
73. Yoganathan S, Bohl TG, Mason G. Plasma cell balanitis and vulvitis (of Zoon). A study of 10 cases. J Reprod Med 1994; 39: 939–944.
74. Sandler B. Sperm basic proteins in cervical carcinogenesis. Lancet 1978; 2: 208–209.
75. Sandler B. Contraceptives and cervical carcinoma. Br Med J 1969; 1: 356–357.
Full text available from CIRP.
Why mice don't live in the foreskins of horses
The article by Boczko and Freed relied heavily on an eccentric experiment from 1947 in which A. Plaut and A. C. Kohn-Speyer tried to induce cancer in mice by doses of smegma harvested from horses. Despite persistent applications, it appears that they were successful in producing cancerous lesions in only about 60 of 400 victims, and I say “appears” because the presentation of their results is so confusing that it is very difficult to work out just what the results were. They also reported that up to 500 days the smegma-treated mice actually fared better than those who missed out: a survival rate of 47% and 30% respectively. Had they stopped the experiment at that point they would have been forced to conclude that horse smegma boosted mouse health. The most one can say about this preposterous exercise is that it explains one of the great puzzles of zoology: why mice don't live inside equine prepuces.
Plaut A, Kohn-Speyer AC. Carcinogenic action of smegma. Science 1947; 105: 391–392.
Circumcision may increase risk of prostate problems
There is no evidence that the presence of the foreskin increases the risk of cancer of the prostate, but recent papers by Dr G.G. Giles et al show that circumcised men experience more prostate problems, and that prostate cancer is not related to STDs.
Prevalence of urinary symptoms in urban Australian men aged 40-69. McCredie M; Staples M; Johnson W; English DR; Giles GG. Department of Preventive and Social Medicine, Dunedin Medical School, University of Otago, New Zealand. J Epidemiol Biostat 2001;6(2):211-8
BACKGROUND: This study was devised to determine the prevalence of urinary symptoms among men living in the Australian cities of Melbourne, Sydney or Perth, and to identify factors associated with the presence of moderate-to-severe urinary symptoms.
METHODS: The study comprised a population-based sample of 1,216 men, aged 40-69 years, whose names were obtained through electoral rolls and who participated as controls in a case-control study of risk factors for prostate cancer. As part of a structured face-to-face interview, the men completed the International Prostate Symptom Score (IPSS). Men with moderate (IPSS = 8-19) or severe (IPSS > or = 20) urinary symptoms were compared with those with mild or no symptoms (IPSS < 8) using unconditional logistic regression.
RESULTS: The age-specific prevalence of moderate-to-severe urinary symptoms (IPSS > or = 8) in men aged 40-49, 50-59, 60-69 years was 16%, 23% and 28%, respectively. Compared with men with no or mild urinary symptoms (IPSS < 8), men with moderate-to-severe symptoms were more likely to report not currently living as married [odds ratio (OR) = 1.5; 95% confidence interval (CI) 1.1-2.0] and being circumcised (OR = 1.5; 95% Cl 1.2-2.0). The increased likelihood associated with drinking an average of > 60g per day of alcohol in the 2 years before interview was of marginal statistical significance (OR = 1.6; 1.0-2.6). There were no significant differences between men with IPSS > or = 8 and those with IPSS < 8 with respect to body mass index, education level, having had a vasectomy, or cigarette smoking.
CONCLUSION: Among Australian men, being circumcised, or not currently living as married, were associated with increased prevalence of urinary symptoms.
Comments
There was no media coverage of this paper, but you can be sure that if the study had, on the contrary, shown that being circumcised was associated with reduced prevalence of urinary symptoms, there would have been newspaper headlines, and the circumfanatics would have been crowing about yet another reason to circumcise baby boys.
How significant are these findings?
Urinary symptoms are often an indication of benign prostatic hyperplasia (BPH). Enlargement of the prostate is a common male ailment, often requiring surgery such as transurethral resection of the prostate (TURP) to improve the sufferer's quality of life. In about 80% of cases, TURP results in infertility (because the semen goes into the bladder rather than being ejaculated) and in 5% to 8% of cases, TURP results in impotence. About 400,000 TURPs are performed annually in the US. If being circumcised increases a man's risk of BPH by 50% (as found in the study above), then if 60% of the at risk population in the US have been circumcised, almost 100,000 of the 400,000 TURPs (25 per cent) were the result of circumcision. Quite apart from the loss of function, think what a waste of surgical resources this represents.
Statistics derived from:
http://www.usrf.org/questionnaires/AUA_SymptomScore.html
http://www.fonendo.com/noticias/9/2001/02/1.shtml
http://www.dva.gov.au/media/publicat/2001/prostate/index.htm
No link between STDs and prostate cancer
In a separate study Giles et al found that prostate cancer was not associated with sexually transmitted diseases, but that it was associated with a low frequency of ejaculations.
Sexual factors and prostate cancer. G.G. Giles, G. Severi, D.R. English, M.R.E. Mccredie, R. Borland, P. Boyle, J.L. Hopper. BJU International, Vol. 92, 2003, 211–216
OBJECTIVE: To assess whether prostate cancer might be related to hormone levels and, by inference, to differences in sexual activity.
PATIENTS, SUBJECTS AND METHODS: In a case-control study of men with prostate cancer aged <70 years at diagnosis and age matched control subjects, information was collected on two aspects of sexual activity; the number of sexual partners and the frequency of total ejaculations during the third to fifth decades of life.
RESULTS: There was no association of prostate cancer with the number of sexual partners or with the maximum number of ejaculations in 24 h. There was a negative trend ( P < 0.01) for the association between risk and number of ejaculations in the third decade, independent of those in the fourth or fifth. Men who averaged five or more ejaculations weekly in their 20s had an odds ratio (95% confidence interval) of 0.66 (0.49–0.87) compared with those who ejaculated less often.
CONCLUSIONS: The null association with the number of sexual partners argues against infection as a cause of prostate cancer in this population. Ejaculatory frequency, especially in early adult life, is negatively associated with the risk of prostate cancer, and thus the molecular biological consequences of suppressed or diminished ejaculation are worthy of further research.
In other words, the Victorians could not have been more wrong: the more ejaculations a man has, the lower his risk of prostate cancer, and the healthier he will be.
No scientific evidence that circumcision reduces the incidence of cancer of the prostate
In a brief commentary published in BJU International in 2007, Brian Morris and two friends claimed that the presence of the foreskin greatly increased the risk of cancer of the prostate, and therefore that mandatory circumcision at birth would save billions of dollars in health costs. In a letter published in reply, Robert Van Howe responds to these extravagant claims.
SIR, The commentary by Morris et al. [1] builds a model for the impact of circumcision on prostate cancer based on three axioms for which there is little or no support. They begin with the notion that prostate cancer is caused by underlying inflammation or infection (possibly sexually transmitted diseases (STDs)), although a link to a specific pathogen remains elusive. This fairly new idea needs further study before basing treatment models on it, especially considering the lack of a correlation between the incidence of prostate cancer and cancer of the cervix, an increase in prostate cancer mortality among Roman Catholic priests, and being inconsistent with other studies [2].
Second, they postulate that uncircumcised men are at greater risk of STDs based on one study, while ignoring the eleven studies that show either no difference or that circumcised men have an overall greater risk of acquiring an STD.
Finally, they postulate that uncircumcised men have a greater risk of prostate cancer based on four studies. Two of these studies are >40 years old and compare the risks of Jews to non-Jews. Prostate cancer incidence varies with race. In the USA, African Americans have nearly twice the risk of Whites, who have twice the risk of Asian Americans [3]. In a study that compared cases of prostate cancer to cases of BPH, circumcised non-Jews had three times the risk of prostate cancer than Jews (Odds ratio (OR) 3.23, 95% CI 1.56–6.69), indicating that Jews, as a racial category, were at lower risk [4]. The other two studies relied on patient report, an unreliable practice, to determine circumcision status.[5,6] The British study failed to consider ethnicity or race, so circumcision status might have been a marker of socioeconomic status [5]. The American study did consider race and found that uncircumcised Blacks had 2.6 times the risk of prostate cancer compared with Blacks circumcised as newborns, while the risk was 1.7 times higher for uncircumcised Whites compared with Whites circumcised as newborns [6].
Their third premise also ignores contrary evidence. In one study, when only non-Jews were considered, uncircumcised men trended towards lower risk of prostate cancer (OR 0.86, 95% CI 0.46–1.58) [7], while in another study no difference was found (OR 0.93, 95% CI 0.55–1.58) [8]. Similarly, no association has been found between PSA levels and circumcision status [9]. If circumcision reduced the risk of prostate cancer, it would be expected that the age-adjusted incidence of prostate cancer would decrease as the circumcision rate increased. In fact, the opposite has been documented [10]. Likewise, if Morris et al. [1] are correct, one would expect the incidence of prostate cancer in Europe to be 36–60% greater than the incidence in the White USA population. For the period 1983–1987, before PSA screening, the age-adjusted incidences of prostate cancer in Denmark, Finland, Iceland, Norway, and Sweden were 48.9, 61.8, 85.0, 71.8, and 81.6 per 100,000, respectively [11]. In 1986 the age-adjusted incidence among USA Whites was 86 per 100,000 [10].
Morris et al. failed to consider race. If Blacks constitute 11% of the USA population and are at twice the risk of prostate cancer, using the racially specific risks the number of cases of prostate cancer by circumcising everyone is 174,997 instead of 167,471. This decreases the estimated cost savings by US$ 125 million.
Morris et al. conveniently chose to not estimate the lost opportunity costs of circumcising 562 704 infants. Using a cost of $195 per circumcision and the standard discount rate of 5% over 70 years, the lost opportunity costs are $3.3 billion, which overwhelms the $1.1 billion in estimated prostate cancer costs.
The concept of using circumcision to reduce prostate cancer risk has no biological or epidemiological foundation. Even if one is willing to depart from reality and use the most extreme assumptions as put forth by Morris et al., circumcision of infants is not cost-effective.
REFERENCES
1. Morris BJ, Waskett J, Bailis SA. Case number and the financial impact of circumcision in reducing prostate cancer. BJU Int 2007; 100: 5–6
2. Giles GG, Severi G, English DR et al. Sexual factors and prostate cancer. BJU Int 2003; 92: 211–6
3. Centers for Disease Control and Prevention. Comparing prostate cancer by race and ethnicity. Available at: http://www.cdc.gov/cancer/prostate/statistics/race.htm. Accessed September 2007.
4. Kaplan GW, O'Connor VJ The incidence of carcinoma of the prostate in Jews and gentiles. JAMA 1966; 196: 123–4.
5. Ewings P, Bowie C. A case-control study of cancer of the prostate in Somerset and east Devon. Br J Cancer 1996; 74: 661–6
6. Ross RK, Shimizu H, Paganini-Hill A, Honda G, Henderson BE. Case-control studies of prostate cancer in blacks and whites in southern California. J Natl Cancer Inst 1987; 78: 869–74
7. Wynder EL, Mabuchi K, Whitmore WF Jr. Epidemiology of cancer of the prostate. Cancer 1971; 28: 344–60
8. Rotkin ID. Studies in the epidemiology of prostatic cancer: expanded sampling. Cancer Treat Rep 1977; 61: 173–80
9. Oliver JC, Oliver RT, Ballard RC. Influence of circumcision and sexual behaviour on PSA levels in patients attending a sexually transmitted disease (STD) clinic. Prostate Cancer Prostatic Dis 2001; 4: 228–31
10. Stanford JL, Stephenson RA, Coyle LM et al. Prostate Cancer Trends 1973–1995, SEER Program, National Cancer Institute. NIH Pub. No. 99-4543. Bethesda, MD; 1999
11. Tretli S, Engeland A, Hadorsen T et al. Prostate cancer – look at Denmark? J Natl Cancer Inst 1996; 88: 128
Robert S. Van Howe,
Case number and the financial impact of circumcision in reducing prostate cancer
BJU International, Vol. 100, Issue 5,1193-1194; published online: 3 October 2007
The most laughable thing about Morris and friends’ eccentric conviction that "lack of circumcision" is a significant risk factor for cancer of the prostate is that the principal support he can muster for this notion is an old article in an obscure journal by an American crackpot called Abraham Ravich. His immortal classic, Preventing VD and Cancer by Circumcision (NY: Philosophical Library, 1973), sits on the curiosity shelves of second hand bookshops along with S.I. McMillen MD, None of these Diseases (Westwood NJ, 1963), in which "a physician testifies that health, happiness and even longer life can be yours if you follow the teaching of the Bible", and Robert B. Greenblatt MD, Search the Scriptures: A Physician Examines Medicine in the Bible (Philadelphia, 1963). Both books confine the Bible to the first few books of the Old Testament, and naturally praise circumcision with all the warmth of Peter Charles Remondino himself. It seems that McMillen's text went through many editions and has been widely distributed and read in the United States, which may help to explain certain peculiarities in the medical culture of that country.
Further information
"Lack of circumcision" not a risk factor for cancer of prostate
Prostate Cancer Foundation of Australia